If you’ve ever been told, “Just sit up straight,” you already know how unhelpful that advice can feel—especially when your body snaps right back into the same position the moment life gets busy. Postural imbalances are rarely about willpower. They’re usually about habit + workload + mobility + strength + your nervous system’s default settings.
In a city like Toronto—where many people bounce between desk time, long commutes, and phone-heavy downtime—posture problems show up in familiar ways: neck tension that won’t quit, mid-back stiffness that makes deep breaths feel shallow, low back flare-ups after sitting, or that nagging “one shoulder higher than the other” feeling.
At Physio Cottage, we look at posture the way it actually behaves in real life: not as a “perfect pose,” but as a moving snapshot of how your body is coping. If you’re searching for physiotherapy scarborough services to address recurring pain that seems tied to your posture, this guide will help you connect the dots—and make a plan that sticks.
What Is a Postural Imbalance?
A postural imbalance is less about “good vs bad” posture and more about how your body distributes load. When some tissues consistently do too much work (tight, overactive, cranky) and others do too little (weak, sleepy, poorly coordinated), your system finds a workaround. That workaround becomes your default posture.
Posture vs. Postural Imbalance (What’s the difference?)
Posture is simply your body’s alignment in a moment—sitting, standing, scrolling, driving, walking.
A postural imbalance is when that alignment becomes predictably biased (same joints compressed, same muscles overused), and it starts affecting:
- movement quality (you move “around” a restriction),
- symptoms (pain, headaches, fatigue),
- function (lifting, running, sleeping, concentration).
In clinic, we often see people who can “stand tall” for 10 seconds… but the moment they reach for a bag, look down at a screen, or take stairs, the old pattern takes over. That’s not laziness; that’s motor control.
Common patterns (Forward head, rounded shoulders, anterior pelvic tilt, etc.)
A few common themes show up again and again:
- Forward head posture: chin pokes forward; upper neck compresses; deep neck muscles underperform.
- Rounded shoulders: shoulder blades tip forward; pecs feel tight; upper back gets stiff.
- Thoracic kyphosis (increased upper-back rounding): often paired with limited extension and restricted ribcage motion.
- Anterior pelvic tilt: pelvis tips forward; hip flexors/low back may feel “tight”; glutes often lag behind.
- Asymmetries: one hip shifts, one shoulder hikes—sometimes related to work setup, past injury, or sport.

Signs Your Posture Is Contributing to Pain or Dysfunction
Not every ache is a posture problem—but posture can quietly turn the volume up on sensitive areas. The giveaway is consistency: symptoms that predictably show up after certain positions (sitting, driving, laptop work, long standing) and ease with movement changes.
Neck pain, shoulder tightness, headaches
This cluster often comes with:
- soreness at the base of the skull,
- upper trapezius “knots,”
- headaches after screen time,
- jaw tension (sometimes).
When the head drifts forward, the neck extensors and upper traps can act like they’re on overtime. Manual techniques can help, but lasting change usually comes from re-training deep neck flexors, scapular control, and better screen habits.
If you’re also exploring massage therapy scarborough options for that tight, banded feeling across the shoulders, it can pair nicely with physiotherapy—especially when massage is followed by targeted strength and control work so the release actually “holds.”
Mid-back stiffness and “tech neck” symptoms
A stiff thoracic spine makes your neck and shoulders compensate. People describe:
- “I can’t sit upright without effort,”
- tightness between the shoulder blades,
- reduced tolerance to desk work.
Often, the fix isn’t forcing your shoulders back; it’s restoring thoracic extension/rotation, ribcage motion, and then integrating that into real tasks (typing, driving, lifting).
Low back pain, hip tightness, glute weakness
Low back pain linked to postural imbalance frequently shows up with:
- tight-feeling hip flexors,
- sore SI joint region,
- glutes that “won’t fire,”
- discomfort after sitting then standing.
A common pattern is the low back doing the job of the hips. The answer is rarely “more core.” It’s usually better hip mechanics + smarter core strategy + graded loading.
For people whose pain has become persistent, you might already be looking into chronic pain treatment scarborough resources. Posture work can be part of that plan—but we’ll keep it practical and grounded in function, not perfection.
Numbness/tingling, fatigue, reduced breathing capacity (when relevant)
Occasional tingling can come from nerve sensitivity, prolonged compression, or irritated tissues. Breathing can also get “stuck” up high in the chest when ribcage and thoracic motion are limited.
Important note: symptoms like progressive weakness, widespread numbness, or changes in coordination deserve prompt assessment (more on this below).
ALso Read: Neck Pain Relief in Scarborough — How Physiotherapy Helps You Heal Faster
How Physiotherapists Assess Postural Imbalances
A good posture assessment isn’t a lecture and a quick glance. It’s a detective job: we look for the driver of the pattern—then test whether changing that driver changes your symptoms and movement.
Health history + symptom mapping
We start with what matters:
- Where do you feel it?
- What triggers it?
- What relieves it?
- What does a typical day look like (work, commute, workouts, sleep)?
This is also where we screen for previous injuries—old ankle sprains and shoulder injuries can quietly shape posture years later.
Movement analysis (squat/hinge/overhead reach/walking)
Static posture is only half the story. We look at:
- squat and hip hinge (do you move from hips or low back?),
- overhead reach (does the ribcage flare? shoulders shrug?),
- gait/walking (pelvis control, trunk rotation),
- simple task simulations (picking up a bag, sitting at a laptop).
Mobility & strength testing (key muscle groups)
We typically check a blend of:
- thoracic mobility (extension/rotation),
- shoulder range (especially flexion/external rotation),
- hip extension and rotation,
- muscle endurance (deep neck flexors, scapular stabilizers),
- glute strength and pelvic control.
Sometimes what feels “tight” is actually a muscle that’s working too hard because something else isn’t doing its share.
Identifying your “driver”: mobility restriction vs weakness vs motor control
This is the hinge point of treatment.
- If mobility is the limiter, we open the range (joints/soft tissue) and then train control in the new range.
- If strength/endurance is missing, we build capacity gradually.
- If motor control is the issue, we practice the pattern until it becomes automatic—like learning a new accent for your movement.
Red flags (when we refer you to a physician/imaging)
Physios don’t ignore warning signs. We’ll refer out if we see signs like:
- progressive neurological weakness,
- bowel/bladder changes,
- unexplained weight loss/fever,
- severe night pain not easing with position changes,
- significant trauma.
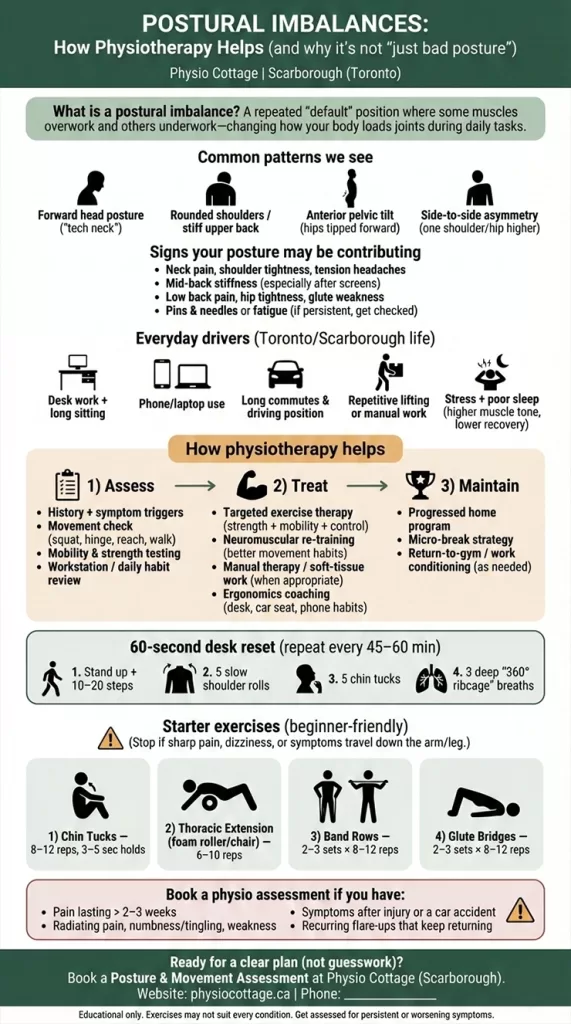
How Physiotherapy Treats Postural Imbalances (The Core Interventions)
Posture improves when your body has options. Treatment is about giving you those options—and making them usable in real life.
Education & habit change (micro-breaks, positions, pacing)
You don’t need a perfect workstation. You need a workstation you can escape regularly.
We often use:
- micro-breaks (30–60 seconds every 30–45 minutes),
- position rotation (chair → standing → walking call),
- symptom rules (what level of discomfort is “okay” vs a sign to modify).
If you want a more whole-person plan that blends pain science, habits, sleep, and graded exposure, that’s where a holistic physiotherapy scarborough approach fits naturally—without drifting into vague advice.
Exercise therapy (strength, mobility, motor control)
This is the main event. We choose exercises that:
- match your pattern (not generic),
- match your life (what you’ll actually do),
- progress sensibly (so it sticks).
A good program often includes:
- thoracic mobility,
- scapular strength (mid/lower traps, serratus anterior),
- deep neck flexor endurance,
- hip extension strength and control,
- breathing mechanics.
Manual therapy (joint/soft tissue techniques—when appropriate)
Hands-on care can help reduce pain, improve short-term motion, and make exercise feel possible.
This is where techniques like myofascial release scarborough style work can be useful—especially when tissues are guarded and you’re stuck in a protective pattern. The key is pairing it with movement retraining so you don’t “reset” and then return to the same overload.
Neuromuscular re-training (re-learning alignment during real tasks)
This is the part many blogs skip.
We practice posture where it matters:
- your typing setup,
- your deadlift/row pattern,
- your work lifts,
- your running mechanics,
- even how you carry your kid or groceries.
Your nervous system learns context. So we train in context.
Ergonomics at work & home (desk, car seat, backpack, pillows)
Ergonomics isn’t about buying fancy gear. It’s about small, high-impact tweaks:
- screen height,
- chair depth and lumbar support,
- keyboard/mouse distance,
- car seat angle and headrest position,
- backpack strap adjustment (both straps, not one).
If you’re unsure which pattern fits you, a visit to a scarborough physiotherapy clinic can save you months of trial-and-error YouTube fixes.
Also Read: Physiotherapy for Back Pain in Scarborough — Effective Treatments That Work
7 Simple At-Home Posture Exercises (Safe, Beginner-Friendly)
These are general options that work well for many common postural imbalances. They’re not a substitute for an assessment—think of them as a safe starting kit.
Chin tucks (deep neck flexors)
A small movement that targets the “support system” at the front of the neck.
How: Sit tall, gently glide your chin straight back (like making a double chin). Hold 3–5 seconds. Repeat 8–12 times.
Good for: tech neck, forward head posture, desk workers.
Skip/modify if: it triggers sharp pain, dizziness, or radiating symptoms—get assessed.
Thoracic extension (foam roller or chair)
When the upper back moves better, the neck and shoulders often relax.
How: Place a foam roller mid-back, support your head, gently extend over the roller. Or use the top of a sturdy chair back. 6–10 slow reps.
Good for: mid-back stiffness, rounded shoulders.
Skip/modify if: you have osteoporosis/vertebral fracture history or this causes sharp rib/back pain.
Scapular retraction / rows
Teaches the shoulder blades to move back and down with control.
How: Band row: pull elbows back, squeeze shoulder blades gently (don’t shrug). 2–3 sets of 8–12.
Good for: rounded shoulders, shoulder ache with desk work.
Skip/modify if: it increases shoulder pinching—check technique or reduce range.
Pec stretch (doorway)
Helpful when the front of the chest feels “short.”
How: Forearm on doorway at shoulder height, step through gently, hold 20–30 seconds, 2–3 rounds.
Good for: tight chest, forward shoulders.
Skip/modify if: you have anterior shoulder instability or numbness/tingling increases.
Hip flexor stretch
Often useful if you sit a lot—done gently and consistently.
How: Half-kneeling, tuck pelvis slightly (think “zip up” the front), shift forward until you feel the stretch in the front of the hip. Hold 20–30 seconds.
Good for: anterior pelvic tilt patterns, low back tightness after sitting.
Skip/modify if: you get pinching in the front of the hip—adjust angle or seek assessment.
Glute bridge / hip hinge drill
A simple way to teach hips to share the workload.
How: Bridge: feet hip-width, squeeze glutes, lift pelvis without over-arching the back. 2–3 sets of 8–12.
Good for: glute weakness, low back overuse.
Skip/modify if: it causes hamstring cramping—reduce height, adjust foot position, or regress.
Breathing drill (ribcage/diaphragm)
Breathing affects ribcage position, neck tone, and core strategy.
How: One hand on belly, one on ribs. Inhale through nose so ribs expand 360° (front/side/back), exhale slowly like fogging a mirror. 5–8 breaths.
Good for: “upper chest breathing,” neck tension, bracing all day.
Skip/modify if: it makes you lightheaded—slow down and keep breaths smaller.

When to See a Physiotherapist (and When It’s Urgent)
If posture changes and home exercises help, great. But if you’re stuck in a loop—pain, brief relief, pain again—a physiotherapist can shorten the path.
Persistent pain > 2–3 weeks
If symptoms keep returning despite rest and basic changes, it’s worth getting assessed. You’ll get clarity on the driver and a plan with progression—so you’re not guessing.
Radiating symptoms, weakness, coordination issues
Seek assessment sooner if you have:
- pain traveling down an arm/leg,
- numbness/tingling that’s persistent or worsening,
- grip weakness, foot drop, balance changes.
After injury, car accident, or return-to-sport concerns
A past injury can change mechanics subtly. After a collision, many people develop protective patterns that look like “bad posture” but are really a guarded nervous system.
If cost, coverage, or navigation is a barrier, ask about community-oriented options such as refugee physiotherapy scarborough programs and supports where applicable—care should be accessible, not intimidating.
Frequently Asked Questions
Can physiotherapy fix posture permanently?
Physio can create lasting change, but “permanent” depends on whether your daily habits and workload keep re-feeding the same pattern. The goal is durable, flexible posture—not rigid perfection.
Is posture correction helpful for scoliosis?
It can help with pain, stiffness, strength, and function. Physiotherapy won’t “erase” structural scoliosis, but it can improve how you move and how symptoms are managed.
Will a posture brace help?
Sometimes short-term—especially as a reminder. But braces don’t build strength or motor control. Most people do better using a brace selectively while building an active program.
How long does it take to improve posture?
Many people feel some relief in 2–4 weeks (with consistency). Visible/postural endurance changes often take 6–12 weeks, depending on workload and starting point.
Do I need imaging (X-ray/MRI)?
Not usually for posture-related pain, unless there are red flags or significant trauma. Most plans start with assessment and conservative care.
Posture Correction in Scarborough/Toronto: How to Get Started
If you’ve read this far, you probably don’t need more generic tips—you need a plan that fits your body and your schedule.
Booking an assessment (what to bring / what we’ll do)
Bring or be ready to discuss:
- your typical work setup (a photo helps),
- what movements trigger symptoms,
- past injuries,
- what you’ve already tried.
In your appointment, we’ll assess movement, mobility, strength, and the real-life tasks that matter to you—then map out a clear progression. If you’re comparing options for physiotherapy scarborough, choose a clinic that measures change and teaches you what to do between sessions.
Call-to-action (Book a physiotherapy assessment)
Ready to stop chasing quick fixes and start building a posture that actually holds up on real Toronto days?
Book a postural imbalance assessment at Physio Cottage (Scarborough) and get a targeted plan—mobility, strength, ergonomics, and practical habits you can keep.








